Today we are going to give you a walk through of a case from a front line physician and his thought process in figuring out how much fluid to give a patient using POCUS. There are many ways to estimate fluid responsiveness/tolerance, some still hotly debated, but I think it’s worthwhile to show what some pit docs are actually doing. Several of the images aren’t that great but it’s more about the thought processes behind them in managing the patient.
Here is Lloyd Gordon’s example:
Often I will see a patient who by my clinical and POCUS assessment is way behind on fluids. I generally look at the JVP, IVC, CVS (? PCE, End diastolic R&L ventricular dimensions, Ventricular contractility), kidneys, IVC, pleura (looking for B lines and effusions), bladder (is there any urine?). Then I take into account the weight and height, the clinical situation and make an educated guess.
This patient was elderly, bordering on morbidly obese, febrile (40.5C), around 5’9″ tall, weak and confused with a productive cough. He had a recent hx of ureteric stone and some interstitial lung disease. His pulse and BP weren’t too bad but he looked toxic. His chest was clear with good A/E. How much fluid to give?
His IVC was pretty well invisible with gas, although after looking where it should have been, I had the impression that it was completely collapsed. The JVP was not visible at 45 Deg.

I checked again supine to make sure there was an internal jugular.
Supine the Jugular appeared as a 1-2 mm thread. At about 10 Deg. head up it disappeared again.
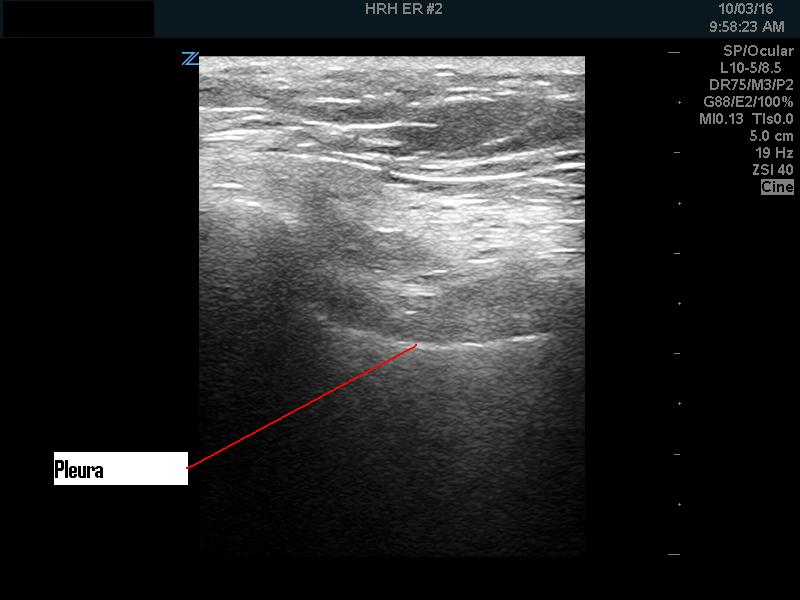
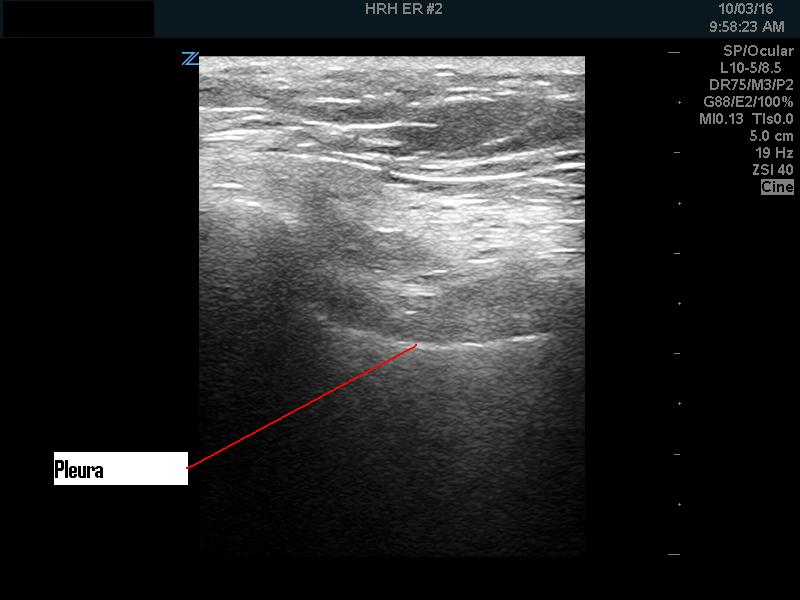
The pleura looked clear with no B lines.
The PSL and Apical 4 Chamber views were pretty bad but after some looking were good enough to pretty well rule out a PCE and see that the R&L ventricles were on the small side and moving reasonably well.


The kidneys looked reasonably good for his age (also no hydronephrosis).


The bladder looked Ok with some urine.
All in all, with the above information, I guestimated that I would order a 3 Liter bolus of NS-> 150cc/hr.
About 30 minutes or so the CXR looked like this (no pulmonary oedema):
Somehow in our ED, “boluses” can take a while. So 2 hours later the RN said that the patient had only 2 L but had “basilar crackles” and so the RN stopped the bolus and went to maintenance and then told me.
I went back, the patient looked much the same. He had urinated only a slight amount. His bladder was a little bigger so he had made some urine (~150 cc).
His pleura looked fine again.

The IVC was still gassed out. However his JVP was now visible and appeared just above the lowest point I could put the probe on the neck (a rather thick neck due to the body habitus).
His chest ,to IPPA, seemed again about the same, reasonably normal for mild interstitial lung disease.
Based on my second clinical and POCUS assessment, I told the RN that the patient was not in pulmonary oedema and to finish off the bolus.
The second CXR confirmed this.
The patient didn’t go into pulmonary oedema later either.
So a reasonably quick assessment with POCUS (say 10 minute tops, probably less, gave a reasonable assessment of fluid needs and the confidence to realize that the bolus would not put the patient into pulmonary oedema.
Like this:
Like Loading...